What the different Korotkov sounds mean.
| Description of sound | Clinical implication | |
|---|---|---|
| Phase I | Appearance of clear tapping sounds | Correlates with systolic blood pressure |
| Phase II | Sounds become softer and longer | No clinical significance |
| Phase III | Sounds become crisper and louder | No clinical significance |
| Phase IV | Sounds become muffled and softer | Correlates as alternate measure of diastolic blood pressure |
| Phase V | Sounds disappear completely | Correlates with diastolic blood pressure |
Capillary circulation
- 5microm in diameter at arterial end and 9microm in venule end
- Minute smooth muscle
- 5% of blood pool at any one time
- At human nail bed arterial end capillary pressure 32mmHg, venous end 15mmHg, transit time 1-2 sec
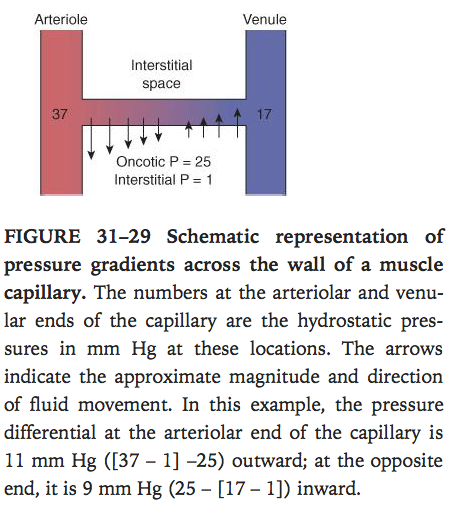
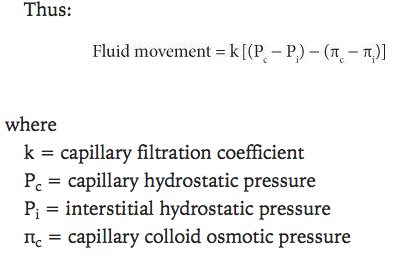
Starling forces & their values. (important).
- The rate of filtration at any point in the capillary is according to the balance of Starling’s forces
- hydrostatic pressure gradient
- Osmotic pressure gradient
- Fluid moves out at arterial end and moves into the vessel at the venous end
Autoregulation (important).
- Autoregulation is the ability of tissues to maintain a stable tissue perfusion at a wide range of blood pressures
- Reflex vasoconstriction of stretched vascular smooth muscle to maintain steady blood flow
- Some metabolites are though to be vasodilators that contribute to this – low flow, these accumulate, vasodilate to increase flow. High flow these metabolites are washed away. (decreased O2, increased CO2, acidosis, high K, lactat, histamine
- Factors affecting auto-regulation
- Prostacyclin(PGI2)
- Prostaglandin that inhibits platelet activation and is a vasodilator
- Thromboxane A2.
- Released from platelets
- Promotes platelet aggregation and potent vasoconstrictor
- EDRF – endothelium derived relaxing factor
- Best known is NO (increase cGMP –> reduce Ca2+ –> smooth muscle relaxation)
- Endothelins:
- Vasoconstrictors mainly released from endothelium
- Hormones:
- Kinins – proteins involved in pain, inflammation, coagulation and BP control eg brady kinin.
- ANP (will be covered later, but be aware of it at this stage).
- ADH (Vasopressin)
- Increased osmolarity sensed in hypothalamus –> ADH release form posterior pituitary –> vasoconstriction (pressin) and increased aquaporins inserted in apical membrane of renal collecting ducts –> increased water reabsorption –> osmolarity reduces.
- Other stimulators of ADH release – angiotensin II, CCK, pain, emotion, surgery
- Inhibitors of ADH release – etOH, ANP
- NA – wk 4 physiology
- Angiotensin II. (see wk 9 pharmacology)
- Nervous regulation: see week 3 physiology
- innervation of blood vessels.
- innervation of the heart.
- the vasomotor centre.
- Prostacyclin(PGI2)
Baroreceptors
- Stretch receptors
- Location – adventitia of carotid sinus, aortic arch, also in LA and RA, pulmonary circulation(cardiopulm receptors)
- Action – afferent signal via glossopharyngeal nerve to medulla –> glutamate–>increase inhibitory tone to vasomotor centre–> increase vagal tone in the balance –> vasodilation, venodilation, bradycardia, drop in BP and decrease CO.
- be familiar (at least in passing) with the reflexes mentioned in the text:
- Bainbridge.
- Bezold-Jarisch.
- Cushing (probably the most askable).
What is the CVS response to a Valsalva ?
4 steps
- Increased intrathoracic pressure
- Reduced venous return–> dec CO and SV
- –> when let go –> initial decreased return to LA due to relaxation of pulm vessels
- increase venous return–> increse CO–> sensed by Baroreceptors –>Increased vagal tone –> Decrease HR and contractility–> decrease CO
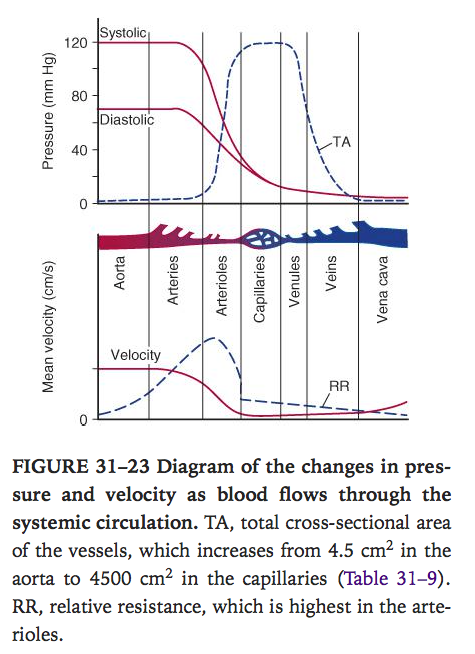
Flow = Pressure/Resistance (in Electricity I = V/R; V=IR)
Laminar flow / turbulent flow.
- Laminar flow is silent, turbulent flow is noisy
- Laminar flow occurs in straight tubes upto a critical velocity then becomes turbulent. Fastest flow is in the centre of the tube.
- Reynold’s number determines the likelihood of turbulent flow
- Porportional to density, diameter of tube, velocity of flow
- Inversely proportional to viscosity
- Reynolds <2000 usually laminar flow, Reynolds>3000 usually turbulent flow
Poiseuille’s Law
- Relationship between flow in a long tube, viscosity and radius
- Physiological significance – flow and resistance vary directly and inversely with r^4, a small change in vessel valibre has a big effect on flow and resistance.
- Flow = pressure difference x r4 x pi/(length of tube x 8 x viscosity)
Laplace’s Law
- Tension in the wall of a cylinder = transmural pressure x radius /wall thickness
- Simplified to P = T/r (wall thickness negligible)
- Explains why a thin wall structure like capillary is not more prone to rupture.
- Smaller the radius of a blood vessel the less pressure in wall required to balance the distending pressure
Vivas
- Tell me about the control of BP
- Baroreceptor response to pressure change
- Starling curve and factors effecting CO
- Effects of Adrenaline/Norad on CO/HR/BP
- Tell me about autoregulation
- Tell me about the control of HR
- What is the CVS response to a Valsalva ?