Week 12 Physiology
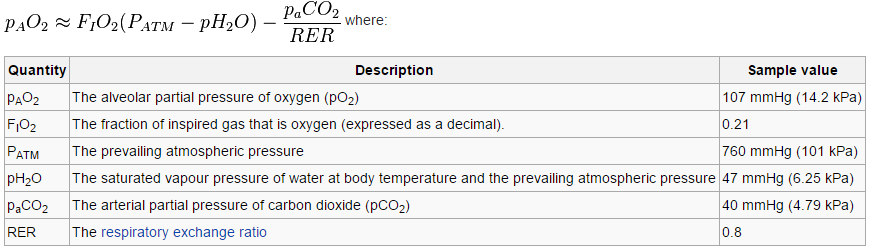
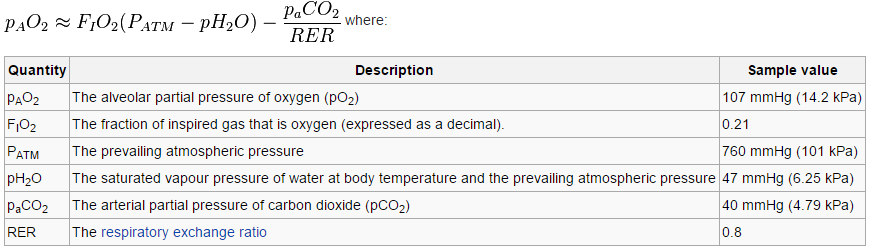
Alveolar gas equation
- PAO2 = PIO2 -PaCO2/R + F
F is correction factor 2mmHG
R is resp ratio between O2 and CO2 diffusion rate, usually 0.8
PAO2= oxygen percentage(atmospheric pressure-47)- (PaCO2 [arterial pressure of cardon dioxide]/0.8)
- Resp quotient
- Fat is 0.7
- Carbohydrates is 1.00
- Brain is 0.97-0.99
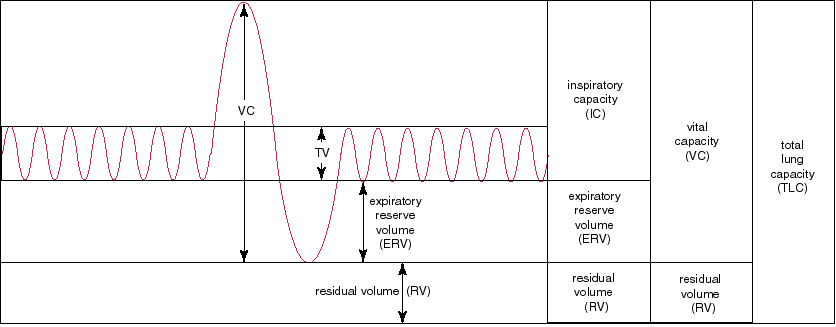
Lung volumes (Important ++)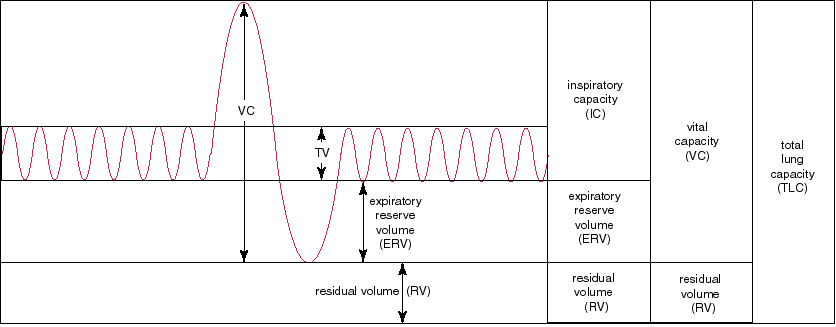
- Tidal volume 500ml – air with each breath entering lung at RR 15 = 7500ml/min(total ventilation)
- Anatomical dead space – air in the conducting airways which don’t participate in gas exchange- approx 150ml
- Alv gas 3l, alv ventilation 5250ml/min
- Pulm blood flow 5000ml/min (70ml cappilary blood)
- Max insp and expiration = vital capacity (6L)
- Remaining gas after max exhalation = residual volume (1.5L)
- Remaining gas after normal exhalation = functional residual capacity(3L)
- TLC = VC + residual volume (7.5L)
- New volume = v1(C1-C2)/C2
- PxV is constant at a constant temperature. So FRC can be measured by body plethysmograph.
- Plethysmograph measures total lung volume even those trapped, helium dilution only measures ventilated volume. The difference can be significant in diseased lung.
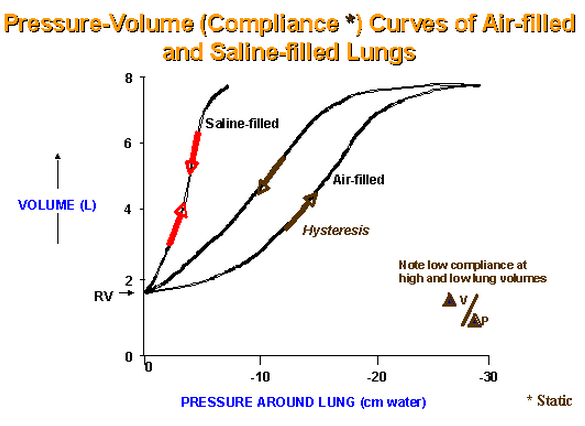
Compliance = change in volume per change in pressure
- More distensible at lower volumes and more stiff and less distensible at high volumes.
- Reduced by fibrosis, alveolar oedema
- Increased with old age, emphysema
Pressure-Volume curves.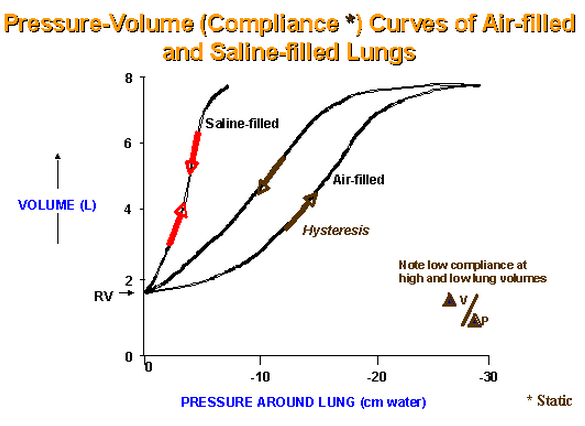
- Hysteresis – the curve that the lung follows during inspiration is different to expiration (pressure – volume curve)
- At any pressure there is more volume in expiration than inspiration (leaf graph)
- At 0 pressure there is some vol due to airway closure and gas trapping- more volume in older people
- Refer to John West for the actual curve
Surfactant.
- Made by alveolar type 2 cells
- Dipalmitylphospholipid
Work of breathing (basic).
Dead space:
- Anatomical – air in the conducting airways which don’t participate in gas exchange- approx 150ml
- Physiological – air that reaches alveoli but doesn’t participate in gas exchange due to lack of perfusion
Other functions of the respiratory system
- Gas exchange, O2 and CO2
- Surfactant production
- Defence – IgA, macrophages
- Filter – pollutants, thromboemboli
- Metabolises some compounds – converts angiotensin 1 to 2, inactivates bradykinin, breakdown prostaglandins and leukotrienes.
- Reservoir for blood
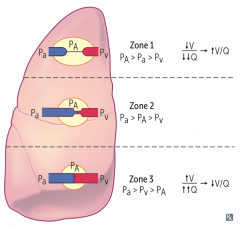
Regional differences in ventilation and blood flow.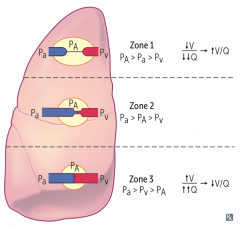
- Distribution of blood in lung
- Decreases almost linearly from bottom to top.
- More blood in dependent areas.
- If ventilated but not perfused = alveolar dead space
- Zone 1 alveolar pressure>arterial>venous
- Zone 2 arterial>alveolar>venous
- Zone 3 arterial>venous>alveolar
- Ventilation of the lung increases as you go more inferiorly – lower lobes of lung are better ventilated than upper zones. Dependent lung is better ventilated.
Muscles of respiration
- Inspiration – diaphragm, external intercostal, SCM
- Expiration – internal intercostal, rectus abdominus, tranverse abdominus,
Review of Poiseuille’s law.
- Flow
- Lamellar flow = (Pressure Difference x pi x radius ^4)/(length of tube x viscosity x 8)
- Whether flow will be laminar or turbulent is predicted using reynolds number = (2xradiusxvelocityxdensity)/viscosity . In straight tube Re has to be over >2000 for probable turbulence.
- Airway resistence is highest in medium sized bronchi
- Dynamic compression – forced expiration- flow is determined by alv pressure minus pleural pressure
Bohr’s equation
- Volume of dead space /tidal volume = (PaCO2-Pexpired CO2) / PaCO2
- Bhors measures physiological dead space (CO2 expired – worse in disease state)=
Diffusion in the lungs.
- Fick’s Law of diffusion
- Amount of gas moving through is proportional to area and inversely proportional to thickness
- V amount = (A/T) x D x pressure or concentration difference. D = sol/root of MW
- Blood travels for 0.75 sec through pulm capillary – if the partial pressure reaches equilibrium before the end and stop diffusing then the agent is perfusion limited cos it has maximally diffused. IF it is still diffusing by end then it is diffusion limited.
- Diffusion capacity increases with exercise.
Pulmonary circulation.
- Pulm artery pressure is 15mmHg (25 to 8)
- Alv cappilaries walls are influenced by the difference between the alveolar pressure and intravascular pressure
- The larger blood vessel’s calibre are affected by lung volume giving traction to their walls.
- V = I R therefore pressure difference = vasc resistance x blood flow.
- Increase in pulm arterial or venous pressure drops the resistance further.
- Recruitment of more capillaries – main
- Distension of already perfused cappilaries at higher pressures.
- Critical opening pressure – the extra alveolar vessels once collapsed require the vascular pressure to be raised above downstream pressure to open due to their intrinsic smooth muscle tone.
- At large lung inflations there Is increased capillary resistance due to increased transmural pressure and reduced calibre of vessels.
- Overall there is a J curve for lung volume vs vasc resistance.
- Seretonin, histamine and acetylcholine increase smooth muscle contraction and increase vasc resistance. Salbutamol and isoproterenol relax airways.
- Ficks principle –> O2 consumption per min = blood flow x concentration difference of O2 at start and end of lung.
- Alveolar hypoxia causes vasoconstriction in small pulmonary arteries
- Non linear – little change when >100mmHg, marked vasoconstriction below 70mmHg
Refer the following topics from Respiratory Physiology by John B West
Chapter 1
- Airways
- Blood vessels
- Initially arteries, veins and bronchi run together but toward the periphery the veins move away and run between lobules.
- Thickness of blood gas barrier is less than 0.3um
- Surfactant
- Reduces surface tension and makes the alveoli more stable at different pressures.
- Dealing with inhaled particles
- Nose filters large particles, small particles deposit in conducting airways – cilia/mucus, smallest go to alveoli – removed by macrophages.
Chapter 2
- Ventilation
- Alveolar ventilation = amount of exhaled Co2 / fraction of Co2 in expired air.
- Fraction of CO2 in alv = partial pressure of Co2 in alv / constant
- Normally PCO2 in alv gas and art blood is equal. So we can figure out alv ventilation using partial pressure of CO2 in arterial blood.
- Fowlers measures anatomical dead space (N2 mixing)
Chapter 9
- Pollutants
- NO2, SO2, ozone, CO, particles, hydrocarbons,
- Placental circulation
- RA to LA via foramen ovale
- Pulm artery to descending aorta via ductus arteriosus
- Placenta is parralel to fetal tissues, whereas adult lung is in series to peripheral tissues
- Fetal PO2 at best (to heart and brain) is 30mmHg, to distal tissue is 22mmHg.
- At first breath the pulm circulation opens, largely assisted by the preinflation of the lungs to 40% by fetal lung liquid(lowers opening pressure req)
Chapter 10
- FEV1, FVC, ratio should be 80%. Low % is obstructive, high% is restrictive
- Lower volume faster drop – restricitive
- Higher volume slower drop – obstructive
- DLCO – for diffusion
- V/Q scan
Viva Questions
- Draw the intrapulmonary / intrapleural pressure curve during respiration.
- Draw a spirometry recording to demonstrate the different lung volumes.
- The wavy one with all the lung volumes TLv, vc, frc, rv etc
- Give me a definition of pulmonary compliance.
- Tell me about the work of breathing.
- Define anatomical and physiological dead space. How do you measure them ?.
- Tell me about regional differences in pulmonary blood flow (or ventilation).
- What is V/Q mismatch ?
- Tell me about the non-respiratory functions of the lung.
- Define surface tension. What is Laplace’s law ? What is the role of surfactant?
- Surface tension
- Laplace’s law (P=2T/r) (for sphere, use 2, for sheet use 4 as numerator)
Explains the tendancy for small alveoli to collapse
- Surfactant – phospholipid, dipalmotoyl phosphatidylcholine- made by type II alveolar cells. Reduces surface tension so increases compliance, decreases collapse of alveoli/APO
- Describe the evolution of the airways from proximal to distal. From what level does gas exchange occur ?
- Trachea–> bronchi–> lobar–> segmental–> terminal(the smallest without alveoli, dust settles) –> resp bronchioles–> alveolar ducts(respiratory zone- diffusion)
- Acinus is lung after terminal bronchiole (2.5-3L)
- After terminal bronchioles there are alveoli – start of gas exchange
- What is the ideal gas equation ?
- PV = nRT
- Pressure x Volume = number of moles x Resp constant x temperature
- Give me a definition of partial pressure.
- In a mixture of gases, each gas has a partial pressure which is the hypothetical pressure of that gas if it alone occupied the volume of the mixture at the same temperature
- Partial pressure of inspired gas = percentage of inspired gas times (total pressure minus water vapour of 47mmHg)
- What is the composition of air ?
- Nitrogen, oxygen, water vapour, inert gases
- Tell me about the muscles of respiration.
- Draw a pressure-volume curve.
- What is diffusing capacity ? How is it measured ?
- Tell me about the pulmonary circulation.
- What is shunting ? Explain physiological shunt.
- Where is the main site of airways resistance ?