| Structure/Class |
- Also known as acetylsalicylic acid.
|
| Pharmacodynamics |
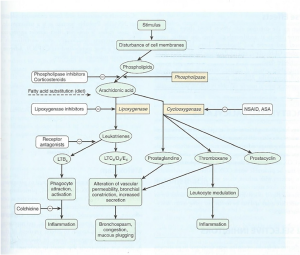
(Diagram retrieved from Katzung 12th edition pg. 639)
- Aspirin is an irreversible inhibitor of platelet COX (this lasts 8-10 days, which is the lifespan of the platelet as the platelet cannot manufacture new COX).
- In other tissues, synthesis of new COX replaces the enzyme so aspirin’s effects on other tissues last 6 to 12 hours.
|
| Absorption/administration |
- PO
- Aspirin is a weak acid with a pKa of 3.5. It is well absorbed in the GIT due to acid pH.
|
| Distribution |
- Aspirin is absorbed in the GIT as ASA. It has a T ½ of 15 minutes (rapidly broken down by red cell esterases). It is hydrolyzed to acetic acid and salicylate. Salicylate is bound to albumin and then undergoes glucuronidation in the liver.
|
| Metabolism |
- At low doses, aspirin follows first order kinetics.
- At higher doses, aspirin follows zero order kinetics. The T ½ is extended to 15 hours.
|
| Excretion |
- It is renally excreted.
- Note that alkalinizing the urine will increase its excretion.
|
| Indications |
- With other drugs that are highly protein bound (e.g. phenytoin).
- It is a weak acid and therefore reduces the clearance of penicillins (like probenacid).
- Decreases the activity of spironolactone.
|
| Contraindications |
|
| Special precautions |
|
| Interactions |
|
| Adverse events |
|
| Dosing/administration |
|
| Toxicology |
- Acute ingestion of >200mg/kg or chronic over medication will cause toxicity.
- The mechanism of toxicity is uncoupling of oxidative phosphorylation and disruption of normal cellular metabolism.
- Signs and symptoms as follows:
- CNS: vertigo, tinnitus and loss of hearing.
- First sign is respiratory alkalosis and hyperventilation. Metabolic acidosis then occurs (usually HAGMA). ABG will show mixed respiratory alkalosis and metabolic acidosis.
- Hyperthermia and vomiting may also occur – contributes to fluid loss and dehydration.
- Severe poisoning leads to profound metabolic acidosis, seizures, coma, pulmonary oedema and cardiovascular collapse.
- Treatment
- Supportive care
- No specific antidote
- Enhanced elimination (activated charcoal, sodium bicarbonate to aid urinary excretion, and haemodialysis if salicylate levels >100)
|
| Withdrawal syndrome |
|
| Special notes |
|